The Procedure
How is it Done?
An initial ultrasound scan of the shoulder is performed. This uses the same sound wave technology used to image a foetus during pregnancy. The high resolution technique can be applied to the shoulder to detect tendon tears or inflammation which could mimic or coexist with frozen shoulder. The ultrasound can also detect inflammation in the lining of the joint which is thought to be implicated in frozen shoulder.
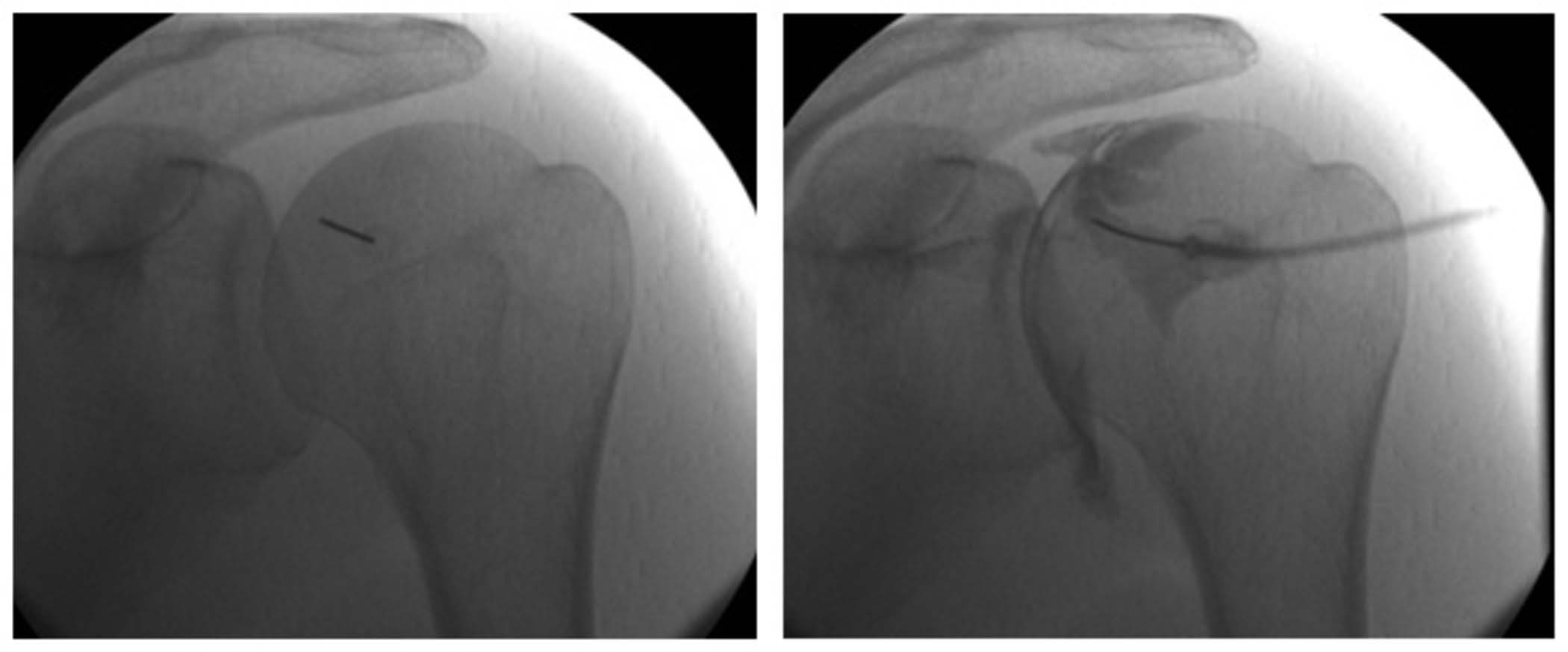
The hydrodilatation is performed in a special X-Ray screening room with the patient lying down. A local anaesthetic is infiltrated to the lining of the joint. A fine needle is positioned in the shoulder joint and the position confirmed with the injection of a small volume of contrast. This is followed by an injection of a long-acting steroid and local anaesthetic. The joint is then further distended with sterile saline.
Patients often experience pain down the arm during the procedure.
The Risks
In our experience, hydrodilatation is very safe.
Some patients are allergic to the iodine-based contrast and may experience a red itchy rash over the area injected. You should inform the radiologist of any previous contrast reactions.
Infection is very rare. If the joint becomes red, swollen and painful or you develop fevers, chills or sweating, you must contact your GP explaining that you have had a joint injection.
The low dose X-Rays provide less radiation dose than a two-hour jet aircraft flight.
Some patients may experience an exaggerated reaction to steroid which can last a few weeks. This is normally self-limiting and can be managed with anti-inflammatory medication.