This Movember, let’s grab the bull by its… horns! Many conditions can affect the male genital area – most are harmless and no cause for concern, whilst others can cause discomfort and may need medical treatment or surgery. Miss Rashmi Singh, Consultant Urological Surgeon at New Victoria Hospital, shares her professional insights on some common male genital conditions, offering professional insights and advice on their diagnosis and treatment. With expertise in General Urology as well as male and female bladder health and kidney stone management, Miss Singh provides a thorough guide to understanding these issues and knowing when to seek help.
An informative look at male genital health
It is well known that men often use humour as a way to broach subjects related to sexual and genital health. This tendency to joke may reflect a reluctance to engage in serious conversations about these topics. Let’s face it: discussing intimate health issues can be awkward for many men. Yet, many conditions are more common than one might think and far from a laughing matter. From “crown jewels” and “net assets” to “down there”, we can name plenty of euphemisms for male private parts, but how well do men actually know their anatomy?
Normal anatomy of the testis
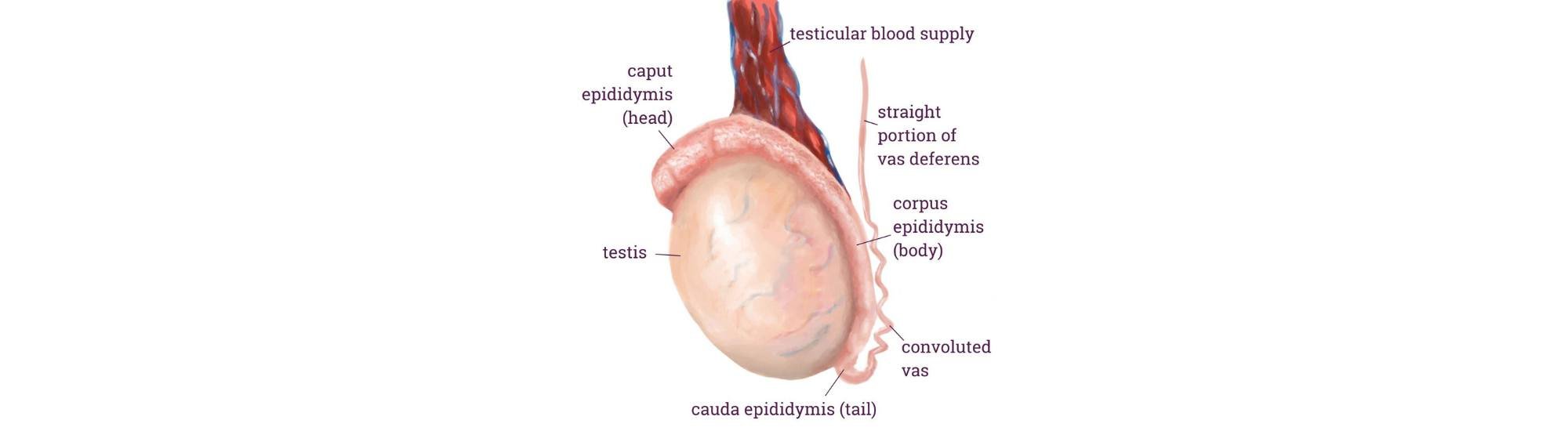
The testicles, or testes, sit outside the body within the scrotal sac, playing a vital role in both reproductive and hormonal health. They produce millions of sperm daily and are also the source of testosterone, the hormone responsible for male characteristics, mood regulation, and libido. Surrounding each testis is the epididymis – a long coiled tube that stores and transports sperm. This structure connects to the vas deferens, a tube that carries sperm to the urethra to mix with fluid to form semen. Together with associated blood vessels and nerves, the vas deferens forms the spermatic cord that links the testes to the inner body.
Various conditions, from testicular torsion to hydrocele and varicocele, can affect these interconnected structures impacting fertility and comfort. In the following sections, we will explore these common conditions, symptoms, and treatments to help demystify the basics of male genital health.
Testicular torsion: when every minute counts
Testicular torsion might sound complex, but it is a straightforward yet painful emergency situation when the spermatic cord twists cutting off blood supply to the testicle. Often affecting young men between ages 12 and 18, this condition can cause sudden, severe pain and swelling. There is a critical treatment window: surgery within 4–6 hours can save the testicle, but waiting longer can result in permanent damage or even loss of fertility.
While there is no new treatment, several national campaigns and case reviews – such as those by The Urology Foundation and NCEPOD – promote symptom awareness and the importance for prompt care, aiming to enhance management practices and improve treatment outcomes for patients.
Epididymal cyst: a common, mostly harmless bump
Found a small, painless lump above the testicle? This could well be an epididymal cyst. These are benign and often discovered during routine exams, though they can grow large enough to be uncomfortable or unsightly. If that is the case, a day case surgical procedure under general anaesthesia can take care of it. Notably, epididymal cysts are often monitored rather than removed unless they cause discomfort. Surgery offers a low recurrence rate and peace of mind for those needing relief.
Varicocele: more than a “bag of worms”
Varicoceles are a form of varicose veins due to swelling of the veins in the spermatic cord. They become more prominent in the standing position and are often described as a “bag of worms”. They are typically harmless but can affect fertility and cause a dull ache, particularly after long periods of standing.
While most varicoceles do not require treatment, those causing pain or impacting fertility, may benefit from embolization – an X-ray procedure that blocks off the main testicular vein without incisions. Recent research also suggests that microsurgical varicocelectomy, a minimally invasive surgical option, offers promising improvements in sperm quality.
Hydrocele: harmless but sometimes annoying
Hydroceles usually have no underlying cause and occur when fluid collects around the testicle, causing a painless swelling. It can occur after an infection or injury to the testis and across all ages, including babies. When they become very large, it can be difficult to feel the actual testis as it sits in a bag of clear fluid, which transilluminates with a torch light.
Though usually benign, they can be bothersome if they become very large. Treatment is a day case surgical procedure to remove the fluid and close off the sac that contained the fluid. The decision whether to treat depends on the size and discomfort it causes.
Epididymoorchitis
Epididymo-orchitis is an infection of the epididymis or testis, typically caused by viral or bacterial urine infections and STDs. Symptoms can develop over a few days and include a tender, swollen, red scrotum with a tender firm testis, fever and generally feeling unwell. In younger men, the condition can mimic testicular torsion, so prompt diagnosis is critical. Early treatment with antibiotics is essential to avoid complications.
Phimosis
Phimosis is a condition where the foreskin is too tight to be pulled back over the glans – the head of the penis – leading to difficulties with urination, self-hygiene and tightness with erections. Balanitis, an infection of the glans can also occur, particularly in patients with diabetes. Primary phimosis is very common in children and for most will resolve with age, but for some it can persist into adulthood. It can also be acquired a result of scarring, infection, or inflammation. Mild cases may be managed with topical steroid creams to loosen the foreskin, but severe cases may require surgery e.g circumcision.
Hernia
An inguinal hernia occurs when a part of an organ, usually intestine, protrudes through a naturally weak spot in the abdominal wall, often causing a noticeable bulge in the groin area that disappears on lying down. The hernia may extend into the scrotum causing more obvious swelling, particularly when standing, lifting, or straining. While hernias are not always painful, they can lead to complications if left untreated. Surgical repair may be recommended to alleviate discomfort, prevent the risk of obstruction or if the hernia is unsightly. Hernia surgery is usually done by General Surgeons not Urologists.
Testicular cancer
First off, here is something encouraging: the rates of testicular cancer are by far lower than many other cancers, including prostate. However, studies show that men, in general, tend to not recognise, downplay, or pay less attention to symptoms and health concerns compared to women, especially in recognising symptoms of conditions like cancer. Early diagnosis is key to positive outcomes, and getting to know what is normal for you and what to look out for can be lifesaving.
Although testicular cancer is not clearly linked to any preventable risk factors, it is still the most common cancer among men aged 20-40. Here are the key signs to watch for:
- A lump or swelling in one of the testicles, often painless
- Discomfort or pain in the testicles or scrotum
- A feeling of heaviness in the scrotum
- A firm, hardened area in the scrotum
- Any change in shape or size between testicles
- Breast enlargement or discharge from the nipples
- A lump in the groin area
When to seek medical advice
If you notice any changes, sharp pain, or that feeling of a “heavy” scrotum, do not put it off. Book a consultation with an Urologist or your GP for a quick check-up. Peace of mind – and health – are worth it.
Regular self-checks are a helpful way to stay on top of your health. If you notice any new swellings, lumps, or other changes in the genital area, do not hesitate to seek medical advice. Often, an examination by your GP or a Urologist, and a simple scan, can rule out any serious issues and give you peace of mind.
To book an appointment with our Urology Consultants, please call us on 020 8949 9020 or fill in our online form.